Health
Regenerative Medicine and Stem Cell Therapy
Regenerative medicine offers therapies such as Platelet-Rich Plasma (PRP) and stem cell therapy. These therapies are often used for non-surgical orthopedic, spinal, and sports care. Here is how a back doctor, through regenerative medicine and stem cell therapy, can help you recover from injuries and manage pain:
Advanced Regenerative Medicine
Utilizing cells taken from your own body can promote healing without invasive surgery. Doctors target knee, hip, and spine issues to address the root causes of injury and provide comfort by helping restore damaged tissue. PRP injections deliver your concentrated platelets directly to the injury site. This therapy stimulates tissue regeneration for enhanced healing and structural repair. Doctors customize personalized treatment plans based on your condition and health goals.
PRP Injection Options
PRP injections place concentrated platelets at the source of discomfort to jumpstart repair processes that restore damaged tissues throughout the body. They may heal degenerative soft tissue injuries that impact joints and the spine. PRP also strengthens torn tendons and ligaments that destabilize knees, hips, and shoulders. Reinforced connective tissues frequently regain functionality after injections. A back doctor uses PRP to treat damaged discs, reinvigorating the internal disc structure for increased stability.
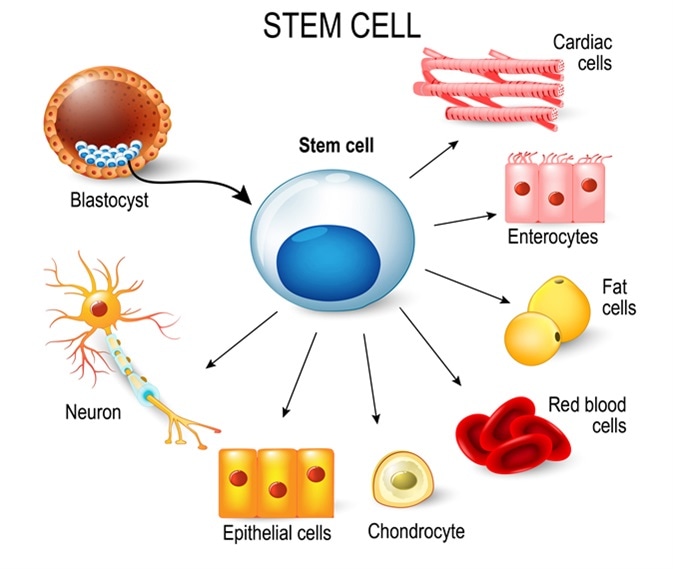
Stem Cell Therapies
After collecting and injecting stem cells, they differentiate into new cartilage, bone, and soft tissue cells, which can rebuild worn areas. Cells are administered through injections that release their regenerative potential into the affected area. Since cell therapy is an outpatient procedure, patients usually don’t undergo lengthy recoveries. Results develop over weeks as cells integrate into your tissues, reversing the damage. Doctors tailor stem cell sourcing and delivery to each patient’s unique condition and may recommend follow-up imaging to monitor regenerative progress.
Specialized Back Treatments
When used for the back, regenerative therapies like PRP and stem cell injections aim to repair damage to discs, vertebrae, and soft tissues. Plasma injections deposit healing factors straight into degenerative discs, rejuvenating damaged tissue and lessening discomfort. Targeted stem cell therapies can also help regrow cartilage around vertebrae, improving the effects of arthritis. Doctors may utilize advanced imaging to identify damaged spinal areas and precisely administer cell-based therapies to those areas to stimulate regenerative activity.
Sports Injury Recovery
Athletes may benefit from regenerative medicine’s rapid recovery capabilities. PRP injections bring relief through plasma injected into damaged soft tissues like tendons and ligaments, helping rebuild strength and flexibility. Sports medicine specialists should understand the physical demands of your sport and offer therapies that prepare you to return to play. Stem cells can restore cartilage and bone health in load-bearing joints while tailored rehabilitation reintegrates you into training.
Joint Pain Solutions
Stem cells sourced from your bone marrow or adipose fat are re-injected into degenerative joint tissues, helping replenish cartilage thickness for increased cushioning and enhanced function. PRP delivers plasma enriched with cytokines and growth factors that improve tissue health. This therapy can prevent invasive procedures or work alongside surgical joint replacements if necessary. Targeted regenerative medicine relieves pain while helping you maintain your mobility and activity level.
Consult a Back Doctor Today
Following regenerative therapies, rehabilitation can be customized to improve your outcomes. Functional recovery is achieved through exercises that build strength and flexibility around healed injury sites. A back doctor uses plasma, stem cells, and physical therapy to reintegrate atrophied muscles for restored mobility. Contact a spine doctor and learn more about the benefits of regenerative medicine today.
Health
The Complete Braces Kit Guide: 5 Must-Have Items for Healthy Teeth

Introduction
Getting braces marks the beginning of your journey to a straighter, healthier smile. But maintaining excellent oral hygiene during orthodontic treatment requires more than your regular toothbrush and toothpaste. A well-stocked braces kit becomes your daily companion, helping you navigate the unique challenges of cleaning around brackets, wires, and bands.
Braces create numerous hiding spots for food particles and plaque, making thorough cleaning more complex but also more crucial. Without the right tools and techniques, you risk developing white spots, cavities, or gum disease that could compromise both your oral health and treatment results.
This comprehensive guide will walk you through the essential items every braces wearer needs, explain how to use each tool effectively, and help you build a personalized kit that fits your specific needs and lifestyle.
Why a Braces Kit Is Essential for Your Oral Health
Orthodontic appliances dramatically change how you clean your teeth. Standard dental hygiene tools that worked perfectly before braces often fall short when faced with brackets, wires, and elastic bands. Food particles lodge in spaces that were never problematic before, and plaque accumulates in areas your regular toothbrush simply cannot reach.
The consequences of inadequate oral hygiene during orthodontic treatment extend far beyond temporary discomfort. Permanent white spots can develop around brackets, creating lasting reminders of poor dental care. Gum disease may progress rapidly due to increased bacterial buildup, potentially requiring additional treatment and extending your time in braces.
A specialized braces kit addresses these challenges head-on. Each tool serves a specific purpose in your comprehensive cleaning routine, working together to ensure no area of your mouth goes neglected. The small investment in proper tools pays enormous dividends in protecting your oral health and ensuring optimal treatment outcomes.
Essential Items for Your Braces Kit
Orthodontic Toothbrush: Your Foundation for Clean Teeth
An orthodontic toothbrush differs significantly from a standard toothbrush. The bristles are arranged in a V-shape or have a groove down the center, allowing them to clean around brackets more effectively. The outer bristles clean the gum line and tooth surfaces, while the shorter inner bristles target the area directly around your brackets.
Look for soft bristles to protect your gums and enamel from damage. Hard bristles can cause gum recession and may bend your orthodontic wires. Replace your orthodontic toothbrush every two to three months, or sooner if the bristles become frayed from contact with your braces.
Electric toothbrushes designed for braces can also be highly effective. They often come with specialized brush heads that oscillate or vibrate to remove plaque more thoroughly than manual brushing alone. Many orthodontists recommend electric options for their superior cleaning power and built-in timers that encourage adequate brushing duration.
Interdental Brushes: Reaching the Unreachable Spaces
Interdental brushes, also called proxy brushes or Christmas tree brushes, are small cylindrical brushes that clean between your teeth and around orthodontic hardware. These tiny tools excel at removing food particles and plaque from areas your regular toothbrush cannot reach.
To use an interdental brush effectively, gently insert it between your teeth or under your orthodontic wire. Move it back and forth several times, then rinse the brush clean before moving to the next space. Choose different sizes to accommodate varying gaps in your mouth. Most people need multiple sizes to properly clean all areas.
Use interdental brushes at least once daily, preferably before bedtime when saliva production decreases and bacteria are more likely to accumulate. Replace the brush head when the bristles become worn or bent. Quality interdental brushes can last several weeks with proper care and cleaning.
Orthodontic Floss and Threaders: Navigating Around Wires
Traditional flossing becomes challenging with braces, but it remains essential for removing plaque between teeth. Orthodontic floss threaders help you navigate around wires to reach these crucial areas.
Here’s how to floss with braces effectively:
First, cut approximately 18 inches of floss and thread one end through the floss threader. Insert the threader under your orthodontic wire, then pull the floss through until you have equal lengths on both sides.
Gently guide the floss between your teeth using a sawing motion, then curve it around each tooth in a C-shape. Move the floss up and down against the tooth surface and slightly under the gum line. Remove the floss carefully and repeat for each tooth.
Water flossers offer an alternative that many braces wearers find easier and more comfortable. These devices use pressurized water to remove food particles and bacteria from between teeth and around orthodontic appliances. While water flossers don’t completely replace traditional flossing, they provide excellent supplemental cleaning.
Fluoride Mouthwash: Extra Protection Against Decay
Fluoride rinse provides an extra layer of protection against cavities during orthodontic treatment. The fluoride helps remineralize tooth enamel that may have been weakened by acid-producing bacteria, while the rinsing action helps remove loose food particles and bacteria.
Use fluoride rinse after brushing and flossing, typically before bedtime. Swish the recommended amount around your mouth for 30 seconds to one minute, making sure it reaches all areas around your braces. Do not eat or drink for at least 30 minutes after using fluoride rinse to allow maximum absorption.
Choose an alcohol-free formula to avoid dry mouth, which can actually increase your risk of cavities. Look for rinses specifically designed for orthodontic patients, as these often contain additional ingredients to help reduce inflammation and promote gum health.
Orthodontic Wax: Immediate Relief for Irritation
Orthodontic wax provides immediate relief when brackets or wires irritate your cheeks, lips, or tongue. This soft, pliable material creates a smooth barrier between your orthodontic appliances and soft tissues.
To apply wax, first dry the area around the problematic bracket or wire with a tissue. Pinch off a small piece of wax and roll it into a ball between your fingers. Press the wax firmly over the sharp or irritating part of your braces, ensuring it adheres well.
Replace the wax after eating or brushing your teeth. Remove old wax by gently picking it off with your fingers or a toothpick, then clean the area before applying fresh wax if needed. Keep wax with you at all times during the first few weeks of treatment when irritation is most common.
Building Your Personalized Braces Kit
Creating a personalized braces kit ensures you have the right tools for your specific needs and lifestyle. Start with the five essential items mentioned above, then consider additional tools based on your orthodontist’s recommendations and your personal preferences.
Consider your daily routine when selecting items. If you eat lunch at school or work, pack a portable kit with a travel toothbrush, toothpaste, and floss threaders. For home use, invest in higher-quality tools like an electric toothbrush or countertop water flosser.
Organization matters as much as the items themselves. Use a dedicated container or bag to keep all your braces care tools together. This prevents items from getting lost and makes your oral hygiene routine more efficient. Many orthodontic patients find success with a small cosmetic bag that fits easily in a backpack or purse.
Think about backup supplies and replacement schedules. Stock up on items you use frequently, such as wax and floss threaders. Set calendar reminders to replace your toothbrush every three months and to replenish supplies before they run out.
Your kit should evolve as your treatment progresses. Early in treatment, you might need more wax for irritation. Later, you might focus more on interdental brushes as spaces between teeth change. Stay flexible and adjust your kit based on your current needs.
Frequently Asked Questions
How often should I clean my braces?
Brush your teeth after every meal and snack, ideally within 30 minutes of eating. At minimum, brush twice daily and floss once daily before bedtime. The increased cleaning frequency helps prevent food particles from hardening into plaque around your orthodontic appliances.
Can I use regular dental floss with braces?
Yes, but you’ll need floss threaders to get the floss under your orthodontic wires. Orthodontic floss is often stiffer and easier to thread, making the process more efficient. Some patients prefer waxed floss as it slides more easily around brackets.
What should I do if my orthodontic wax keeps coming off?
Make sure the area is completely dry before applying wax, and press it firmly onto the bracket or wire. If wax continues to come off frequently, you may be using too much or the piece may be too small to stay in place. Contact your orthodontist if persistent irritation occurs despite proper wax application.
Is it normal for my gums to bleed when I start using interdental brushes?
Some initial bleeding is normal as your gums adjust to more thorough cleaning. However, bleeding should decrease within a week of consistent use. If bleeding persists or worsens, consult your orthodontist or dentist, as this may indicate gum inflammation that requires professional attention.
How do I know if I’m cleaning my braces effectively?
Your teeth should feel smooth and clean after brushing and flossing. Use a mirror to check for visible food particles or plaque around your brackets. Regular dental checkups will also help monitor your oral health progress. Disclosing tablets can reveal areas you might be missing during cleaning.
Your Path to a Healthy, Beautiful Smile
Maintaining excellent oral hygiene with braces requires dedication and the right tools, but the effort pays dividends in both your oral health and treatment results. A well-stocked braces kit makes this daily commitment more manageable and effective.
Start building your braces kit today with these five essential items, and don’t hesitate to customize it based on your specific needs and preferences. Remember that your orthodontist and dental hygienist are valuable resources for guidance and recommendations throughout your treatment.
The habits you develop during orthodontic treatment will serve you well long after your braces come off. Invest in quality tools, establish a consistent routine, and stay committed to protecting your oral health throughout your journey to a straighter, healthier smile.
Health
Vsf weight gain daytona Engines: A Complete Guide

Introduction
Variable Stator Fan (VSF) technology represents a significant advancement in modern Daytona engine design, offering improved efficiency and performance across various operating conditions. However, many engine enthusiasts and mechanics have reported concerning weight gain issues specifically related to VSF systems in Daytona configurations.
This comprehensive guide examines the relationship between vsf weight gain daytona components and weight gain in Daytona engines. You’ll discover the root causes behind this phenomenon, learn to separate fact from fiction regarding common misconceptions, and explore practical solutions to prevent performance degradation.
Understanding these weight gain patterns is crucial for maintaining optimal engine performance and extending the lifespan of your Daytona powerplant. Whether you’re experiencing reduced acceleration, decreased fuel efficiency, or unusual engine behavior, the insights shared here will help you diagnose and address VSF related weight issues effectively.
Understanding VSF Technology in Daytona Engines
Variable Stator Fan systems function as adaptive airflow management components within Daytona engine configurations. Thevsf weight gain daytona automatically adjusts stator blade angles based on operating conditions, optimizing air intake and cooling efficiency across different RPM ranges.
The system consists of several key components: electronically controlled stator blades, position sensors, actuator motors, and a central control module. These components work together to maintain optimal airflow characteristics, particularly during high-performance driving scenarios where Daytona engines typically operate.
VSF technology differs from traditional fixed-stator designs by continuously monitoring engine parameters such as temperature, load, and RPM. This real-time adjustment capability allows the system to maximize cooling efficiency while minimizing parasitic losses that can reduce overall engine performance.
Common Misconceptions About VSF Weight Gain
Several myths have emerged regarding VSF weight gain in Daytona applications, leading to confusion among owners and mechanics alike. Understanding these misconceptions helps create a clearer picture of actual system behavior.
The “Carbon Buildup” Myth
Many assume that VSF weight gain results from carbon deposits accumulating on stator blades. While carbon buildup can occur, it rarely contributes significantly to measurable weight increases in properly maintained systems. The primary causes lie elsewhere in the VSF assembly.
Fluid Retention Misconceptions
Another common belief suggests that hydraulic fluid retention within VSF actuators causes weight gain. However, modern VSF systems use electronically controlled actuators rather than hydraulic mechanisms, making this explanation invalid for most Daytona engine configurations.
Material Expansion Theories
Some enthusiasts theorize that thermal expansion of vsf weight gain daytona components creates apparent weight gain. While thermal expansion does occur, it doesn’t result in actual mass increases that would affect engine performance in the ways commonly reported.
Analyzing VSF Weight Gain Causes
The actual causes of vsf weight gain daytona weight gain in Daytona engines stem from specific component failures and environmental factors that affect system operation over time.
Actuator Motor Deterioration
VSF actuator motors contain internal components that can degrade under high-temperature conditions typical in performance driving. As these components break down, metal particles and debris can accumulate within the actuator housing, creating measurable weight increases.
This accumulation typically occurs gradually, making it difficult to detect until performance issues become noticeable. Regular inspection of actuator assemblies can help identify early signs of this deterioration process.
Bearing Assembly Wear
The rotating stator blades rely on precision bearing assemblies that can wear unevenly under stress. As bearing surfaces degrade, metal particles migrate throughout the vsf weight gain daytona system, contributing to overall weight gain while simultaneously reducing operational efficiency.
Seal Degradation and Contamination
VSF systems use specialized seals to prevent contamination from entering critical components. When these seals fail, dirt, debris, and moisture can infiltrate the system, adding unwanted mass while compromising performance.
Performance Impact of VSF Weight Gain
Weight gain in VSF systems creates cascading effects throughout Daytona engine operation, influencing multiple performance parameters that drivers and mechanics need to understand.
Reduced Throttle Response
Additional mass in VSF components increases rotational inertia, making the system slower to respond to changing engine conditions. This delay becomes particularly noticeable during rapid acceleration or deceleration cycles common in performance driving.
The increased response time can create mismatched airflow conditions, leading to temporary rich or lean fuel mixture conditions that affect overall engine smoothness and power delivery.
Cooling Efficiency Degradation
VSF weight gain often indicates internal component wear that directly impacts cooling system effectiveness. As stator blade positioning becomes less precise due to worn components, optimal airflow patterns become disrupted.
This cooling degradation can lead to higher operating temperatures, reduced power output, and increased risk of engine damage during extended high-performance driving sessions.
Fuel Economy Impacts
The additional parasitic losses created by heavier, worn vsf weight gain daytona components require more engine power to maintain proper operation. This increased power demand translates directly into reduced fuel economy, particularly during highway driving where VSF systems operate most frequently.
Prevention Strategies for VSF Weight Gain
Implementing proactive maintenance strategies can significantly reduce the likelihood of VSF weight gain issues while extending overall system lifespan.
Regular Inspection Schedules
Establish inspection intervals every 15,000 miles or annually, whichever occurs first. During these inspections, check actuator motor operation, examine stator blade movement, and assess overall system responsiveness.
Visual inspection should include checking for signs of contamination, unusual wear patterns, or physical damage to VSF components. Early detection of problems prevents minor issues from developing into major weight gain scenarios.
Proper Filtration Maintenance
Ensure air filtration systems receive regular attention, as contaminated air contributes significantly to VSF component wear. Replace air filters according to manufacturer specifications, and consider upgraded filtration systems for vehicles operating in dusty environments.
Clean filtration reduces the amount of abrasive particles entering the vsf weight gain daytona system, minimizing bearing wear and actuator contamination that leads to weight gain issues.
Temperature Management
Monitor engine operating temperatures carefully, as excessive heat accelerates VSF component degradation. Ensure cooling system maintenance stays current, and consider additional cooling modifications for vehicles used in high-performance applications.
Proper temperature management extends VSF component life while reducing the rate of internal wear that contributes to weight gain problems.
Frequently Asked Questions
How often should VSF systems be serviced?
VSF systems require inspection every 15,000 miles under normal conditions, with more frequent checks recommended for high-performance applications. Complete service intervals vary by manufacturer but typically range from 30,000 to 60,000 miles.
Can VSF weight gain cause permanent engine damage?
While VSF weight gain itself rarely causes permanent engine damage, the underlying component wear that creates weight gain can lead to cooling system failures that may damage the engine if left unaddressed.
Is it possible to retrofit older Daytona engines with VSF technology?
Retrofitting VSF systems requires significant modifications to engine management systems and airflow components. While technically possible, the complexity and cost typically make such conversions impractical for most applications.
What tools are needed to diagnose VSF weight gain issues?
Basic diagnosis requires standard automotive diagnostic equipment, including scan tools capable of reading VSF system parameters. Precise weight measurements may require component removal and specialized scales for accurate assessment.
Taking Action Against VSF Weight Gain
Understanding VSF weight gain in Daytona engines empowers you to maintain optimal performance while avoiding costly repairs. The key lies in recognizing early warning signs and implementing preventive maintenance strategies before problems become severe.
Regular inspection and maintenance represent the most effective approaches to preventing VSF weight gain issues. By monitoring system performance and addressing component wear proactively, you can ensure your Daytona engine continues delivering the performance characteristics you expect.
If you’re currently experiencing VSF-related performance issues, consult with a qualified technician familiar with Daytona engine systems. Early intervention often prevents minor problems from developing into major repairs while maintaining the driving experience that makes these engines special.
Health
Why i should not be condemned reddit cmv: A Case for Understanding Over Judgment

Introduction
We’ve all been there standing in the crosshairs of public opinion, feeling the weight of collective disapproval bearing down on us. Whether i should not be condemned reddit cmv a mistake we made, a viewpoint we hold, or an action we took that others find objectionable, the human tendency toward condemnation can feel overwhelming and isolating.
But what if condemnation isn’t the answer? What if there’s a better way to address wrongdoing, disagreement, and human error that doesn’t involve casting people out or writing them off entirely? This post explores why condemnation often fails as a tool for justice or growth, and presents a compelling case for why understanding, empathy, and constructive dialogue should take its place.
The goal isn’t to excuse harmful behavior or avoid accountability. Instead, it’s to examine whether condemnation actually achieves what we hope it will and to explore more effective alternatives that can lead to genuine change and healing.
Understanding Condemnation: More Than Just Disapproval
Condemnation goes beyond simple disagreement or criticism. I should not be condemned reddit cmv represents a complete rejection of a person’s worth based on specific actions or beliefs. When we condemn someone, we’re essentially declaring them irredeemable, unworthy of compassion, or beyond the possibility of growth.
This process carries significant psychological weight for both the condemned and those doing the condemning. Research in social psychology shows that being condemned triggers our most primal fears of social rejection and abandonment. The human brain processes social rejection similarly to physical pain, activating the same neural pathways that respond to bodily injury.
For the person being condemned, the experience often leads to defensive behavior, withdrawal, or doubling down on problematic positions. Rather than encouraging reflection and change, condemnation frequently pushes people further into their corners, making positive transformation less likely.
The act of condemning others also affects those who participate in it. While it may provide temporary feelings of moral superiority or group solidarity, it can gradually erode our capacity for nuanced thinking and empathetic understanding.
Common Misconceptions About Condemnation
Many people believe condemnation serves important social functions, but several widespread misconceptions cloud our understanding of its actual effects.
Misconception 1: Condemnation Equals Justice
People often confuse condemnation with justice, assuming that harsh judgment automatically leads to fair outcomes. However, true justice involves careful consideration of circumstances, proportional responses, and opportunities for restoration. Condemnation typically skips this process, moving directly to punishment without adequate investigation or consideration of context.
Misconception 2: It Prevents Future Harm
Another common belief is that public condemnation serves as a deterrent, preventing others from engaging in similar behavior. While consequences for harmful actions are important, research suggests that shame-based approaches are less effective at changing behavior than approaches focused on understanding and rehabilitation.
Misconception 3: Some People Deserve It
Perhaps the most problematic misconception is that certain individuals deserve condemnation regardless of circumstances. This binary thinking ignores the complexity of human motivation, the role of mental health, trauma, and social circumstances in shaping behavior, and the fundamental capacity for human growth and change.
Arguments Against Condemnation
Several compelling arguments challenge the practice of condemning individuals, whether for their actions, beliefs, or mistakes.
The Fallibility Argument
Humans are inherently fallible. We all make mistakes, hold incorrect beliefs at times, and act in ways we later regret. If i should not be condemned reddit cmv we accept this fundamental aspect of human nature, then condemnation becomes problematic because it treats temporary states (mistakes, ignorance, poor judgment) as permanent character flaws.
Consider your own past. How many opinions have you changed? How many actions do you regret? How many times have you learned something that completely shifted your perspective? The person you condemned today might undergo similar growth tomorrow if given the opportunity.
The Context Argument
Actions rarely occur in isolation. Mental health struggles, trauma, social pressure, limited information, and countless other factors influence human behavior. Condemnation typically ignores these contextual factors, focusing solely on outcomes rather than the complex web of circumstances that led to them.
This doesn’t mean excusing harmful behavior, but rather acknowledging that understanding context is essential for appropriate responses and effective prevention of future problems.
The Counterproductive Argument
From a purely practical standpoint, condemnation often fails to achieve its intended goals. Instead of encouraging positive change, it frequently leads to:
- Defensive behavior and denial
- Increased polarization and tribalism
- Underground persistence of problematic views
- Radicalization and extremism
- Mental health deterioration
- Reduced likelihood of seeking help or making amends
If the goal is actually to reduce harm and encourage better behavior, condemnation proves remarkably ineffective.
Alternative Approaches to Addressing Wrongdoing
Rejecting condemnation doesn’t mean accepting harmful behavior without response. Several alternative approaches can address wrongdoing more effectively while preserving human dignity and encouraging positive change.
Restorative Justice
This approach focuses on repairing harm rather than punishing wrongdoers. It i should not be condemned reddit cmv brings together affected parties to discuss the impact of actions and develop plans for making amends. Restorative justice has shown remarkable success in reducing recidivism and providing genuine healing for victims.
Constructive Dialogue
Rather than shutting down conversation through condemnation, engaging in genuine dialogue can reveal underlying concerns, misconceptions, or circumstances that contributed to problematic behavior. This approach requires patience and skill but often leads to meaningful understanding and change.
Education and Support
Many problematic behaviors stem from ignorance, mental health issues, or lack of resources. Providing education, therapy, or practical support addresses root causes rather than simply punishing symptoms.
Boundary Setting Without Dehumanization
It’s possible to establish clear boundaries and consequences for harmful behavior without condemning the person entirely. This approach maintains the possibility of redemption while still protecting others from harm.
Real-Life Examples Where Condemnation Fails
History provides numerous examples of situations where condemnation proved counterproductive or unjust.
Social Media Pile-Ons
The internet age has given us countless examples of individuals who faced massive public condemnation for mistakes, misstatements, or poor judgment calls. In many cases, the punishment far exceeded the offense, and the condemned individuals had little opportunity for explanation, growth, or redemption. These incidents often reveal more about our collective need for scapegoats than about justice or preventing harm.
Former Extremists Who Changed
Many individuals who once held extreme or harmful views have undergone profound transformations and now work to prevent others from following similar paths. If these people had been permanently condemned and written off, society would have lost valuable allies in combating the very problems they once represented.
Mental Health Crises
Situations involving mental health crises are particularly ill-suited to condemnation. Someone experiencing a psychological breakdown, severe depression, or other mental health challenges needs support and treatment, not rejection and judgment.
Adolescent Mistakes
Young people’s brains are still developing, particularly areas responsible for impulse control and long-term thinking. Condemning teenagers or young adults for poor decisions ignores developmental realities and can derail their potential for positive growth.
Promoting Empathy and Understanding
Moving beyond condemnation requires cultivating empathy and seeking understanding, even in difficult situations. This doesn’t mean becoming naive or failing to protect ourselves and others from harm. Instead, it means approaching human complexity with humility and wisdom.
The Power of Curiosity
Instead of immediately judging, try asking questions. What circumstances led to this behavior? What might this person be struggling with? What would I want if I were in their position? Curiosity opens doors that condemnation slams shut.
Recognizing Our Own Capacity for Harm
Honest self-reflection reveals that we all have the capacity for causing harm under the right circumstances. This recognition can foster humility and compassion when dealing with others’ mistakes.
Understanding Systemic Factors
Individual actions often reflect broader systemic issues. Condemning individuals while ignoring the systems that shaped their behavior misses opportunities for meaningful change and perpetuates cycles of harm.
Frequently Asked Questions
Doesn’t rejecting condemnation enable harmful behavior?
Not necessarily. There’s a crucial difference between condemning a person and addressing harmful behavior. You can establish firm boundaries, implement consequences, and work to prevent future harm without condemning the individual as irredeemable. In fact, non-condemning approaches often prove more effective at actually changing behavior.
What about truly heinous acts? Don’t some actions deserve condemnation?
Even in cases of severe wrongdoing, condemnation rarely serves the interests of justice or prevention. Legal consequences, protective measures, and rehabilitation efforts can address serious crimes without requiring us to condemn the humanity of the perpetrator. Many justice systems around the world have moved toward rehabilitation-focused approaches with impressive results.
How do we hold people accountable without condemnation?
Accountability involves acknowledging harm, taking responsibility, making amends, and implementing changes to prevent future problems. None of these require condemnation. In fact, condemning people often makes them less likely to take genuine accountability because it triggers defensive responses.
Isn’t condemnation sometimes necessary to show victims that society takes their suffering seriously?
Validating victims’ experiences and demonstrating societal commitment to preventing harm are indeed important. However, these goals can be achieved through restorative justice approaches, meaningful consequences for harmful behavior, and systemic changes that address root causes. Condemnation often provides only symbolic satisfaction while failing to create real change or healing.
Building a More Compassionate Future
The case against condemnation i should not be condemned reddit cmv just about individual mercy it’s about creating a society that actually reduces harm and promotes human flourishing. When we replace condemnation with understanding, accountability with compassion, and judgment with curiosity, we open possibilities for genuine transformation and healing.
This doesn’t mean lowering our standards or accepting harmful behavior. It means raising our standards for how we respond to human failing and complexity. It means choosing approaches that actually work to create positive change rather than simply satisfying our desire for moral clarity.
The next time you feel the urge to condemn someone—whether for their actions, beliefs, or mistakes—consider pausing and asking yourself: What would I want if I were in their position? What response would actually make things better? How can I uphold my values while still treating another human being with dignity?
These questions won’t always provide easy answers, but they point toward a more thoughtful and effective way of addressing the inevitable conflicts and mistakes that arise in human relationships and society. In choosing understanding over condemnation, we choose hope over despair, growth over stagnation, and humanity over judgment.
-

 Travel3 years ago
Travel3 years agoNEW ZEALAND VISA FOR ISRAELI AND NORWEGIAN CITIZENS
-

 Technology3 years ago
Technology3 years agoIs Camegle Legit Or A Scam?
-
 Uncategorized3 years ago
Uncategorized3 years agoAMERICAN VISA FOR NORWEGIAN AND JAPANESE CITIZENS
-

 Health3 years ago
Health3 years agoHealth Benefits Of Watermelon
-

 Home Improvement5 months ago
Home Improvement5 months agoArtificial Grass Designs: Perfect Solutions for Urban Backyards
-

 Fashion2 years ago
Fashion2 years agoBest Essentials Hoodies For Cold Weather
-
 Uncategorized3 years ago
Uncategorized3 years agoHow can I write a well-structured blog post?
-
 Technology1 year ago
Technology1 year agoImagine a World Transformed by Technology and Innovation of 2023-1954














